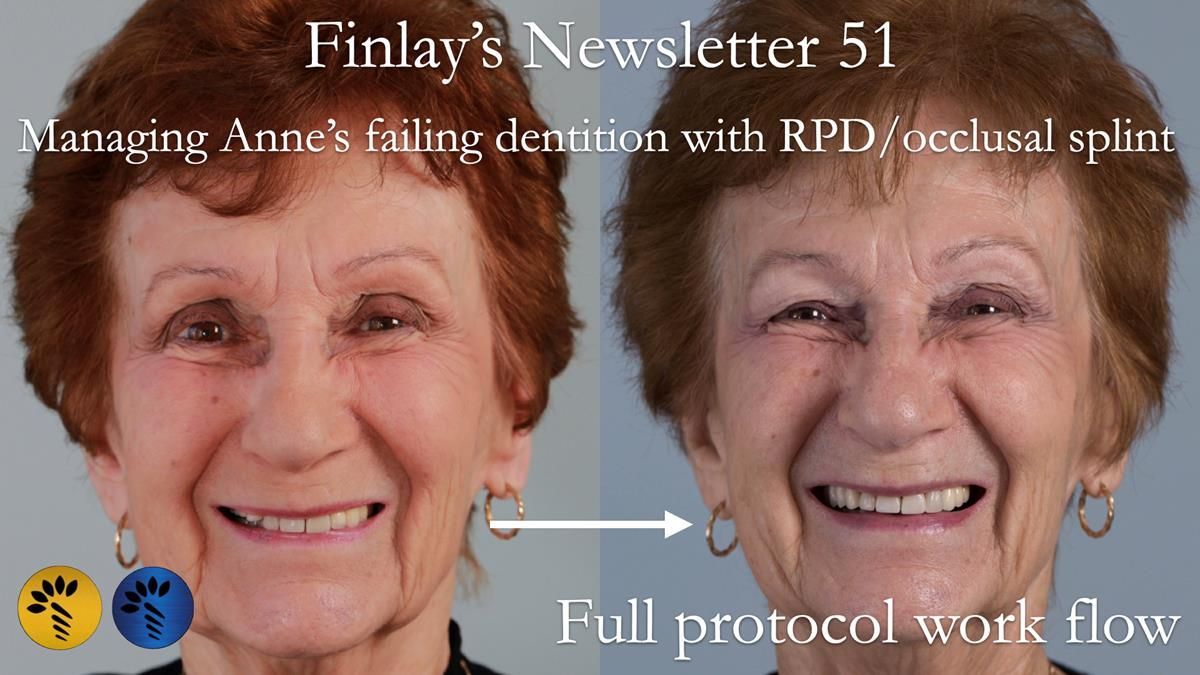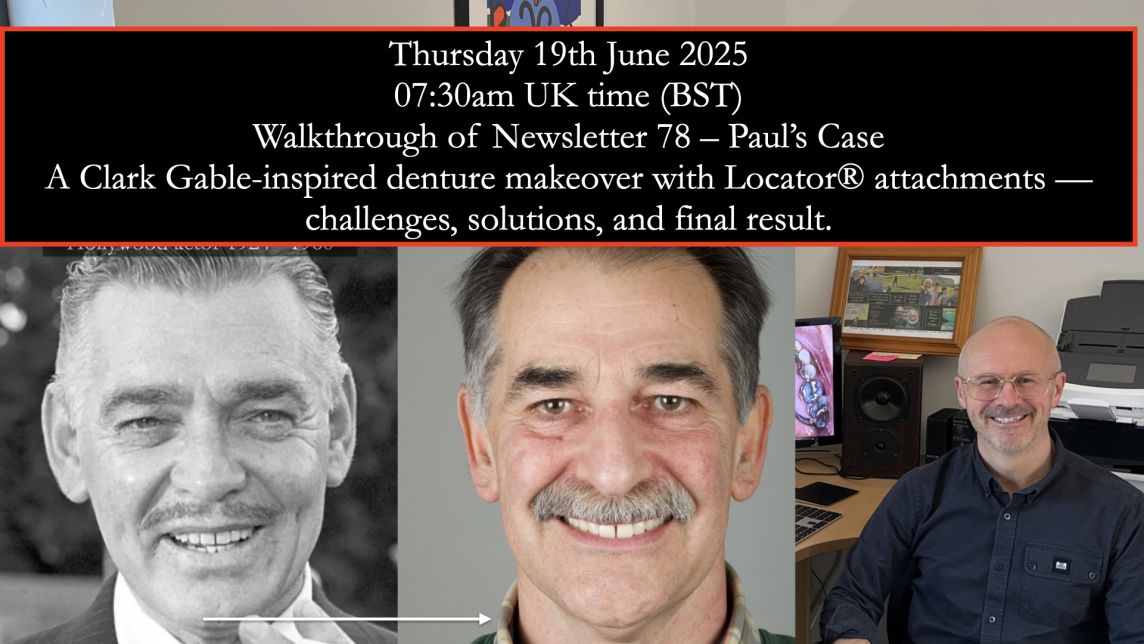
Finlay's Case Presentation
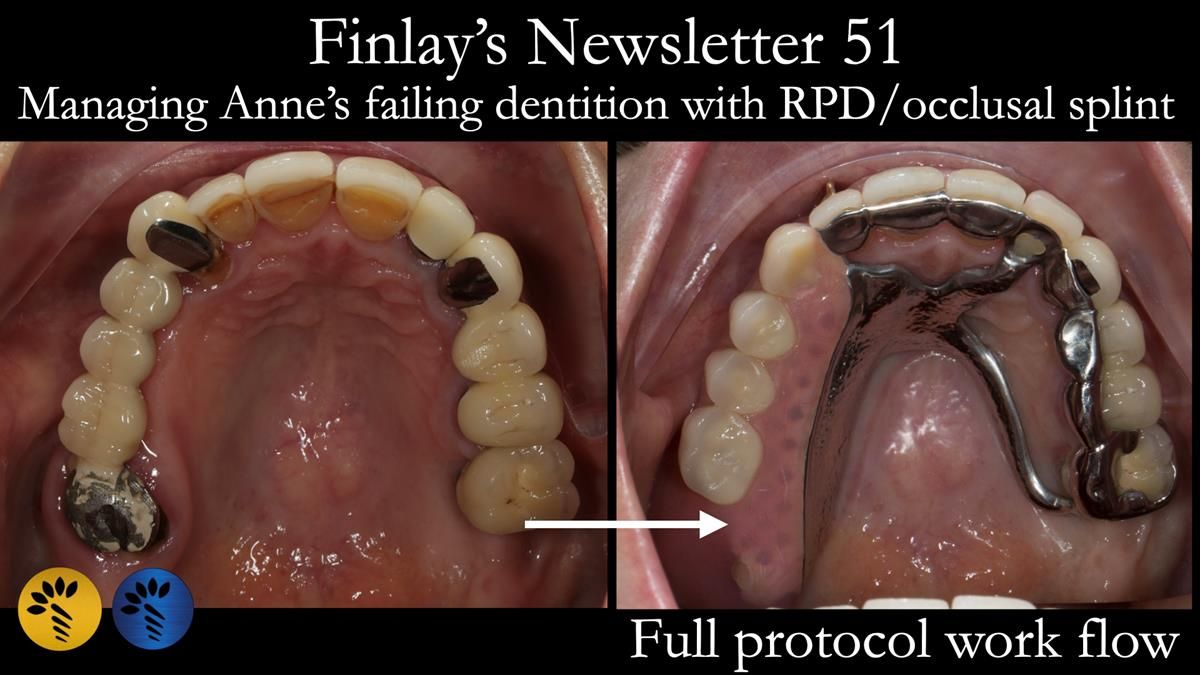
Welcome to Newsletter 51 Case Presentation.
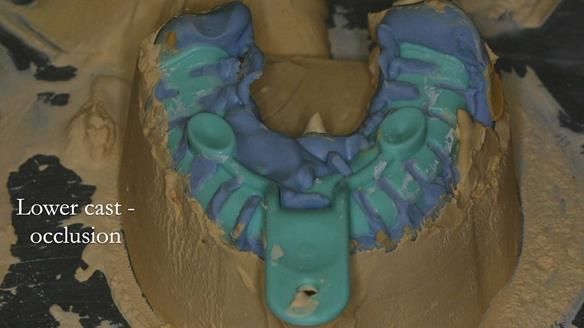
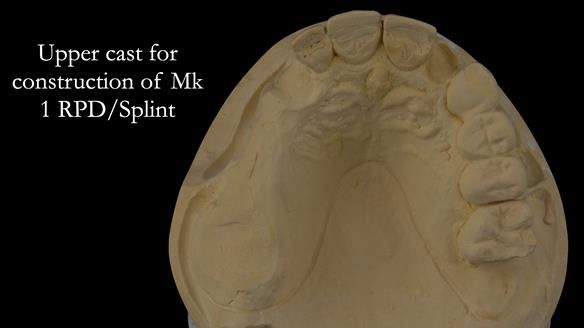
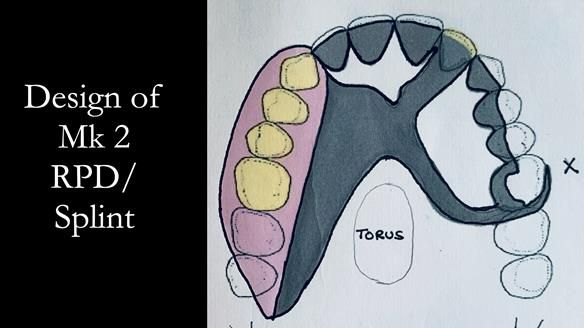
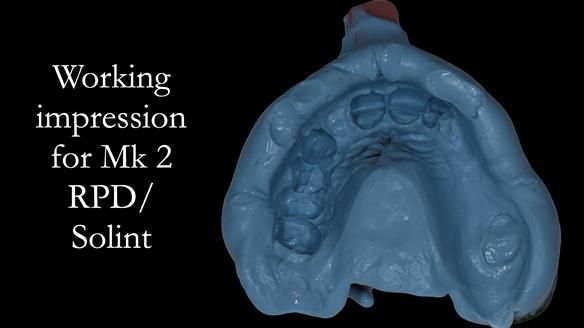
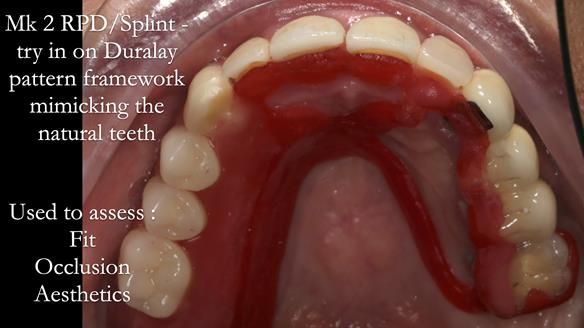
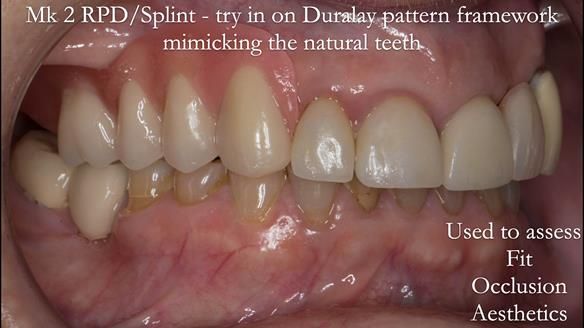
This newsletter describes in step-by-step detail Anne’s treatment stages to provide a metal based removable partial denture/occlusal stabilisation splint to resolve missing teeth and TMJ pain.
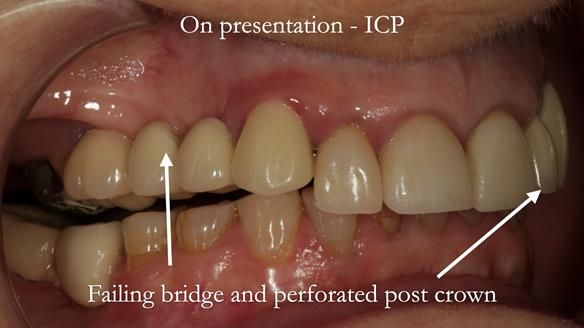
This 75-year-old woman was referred to me by her general dental practitioner.
Dental history prior to treatment
- Temporomandibular Pain Dysfunction Syndrome
- Implant failure
- Heavily restored dentition
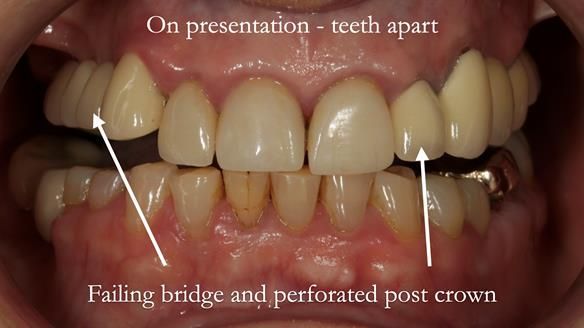
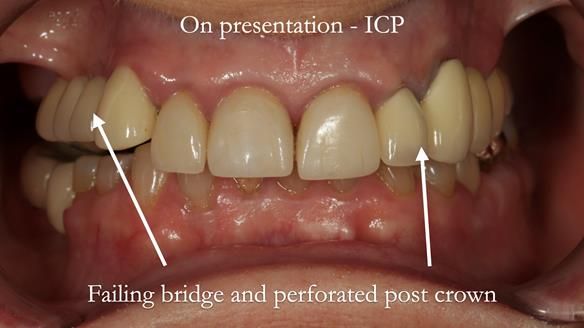
Presenting problems and concerns with the teeth
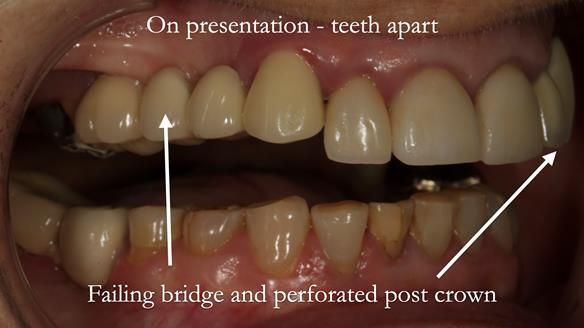
- “Only place to chew is the left-hand side”.
- “Upper right bridge is loose and misplaced. This is a constant worry as it may drop out at any stage.”
- “I can now bite on the front teeth and am concerned that the veneers on the upper front teeth may be overloaded and break.”
- “I have a bite guard you protect the teeth at night.”
- “I grind my teeth during the day and night.”
- “Soreness and pain in jaw joints and face.”
- “I do not want to have further dental implant treatment. One failed in the upper left part of my mouth.”
Dental wish list
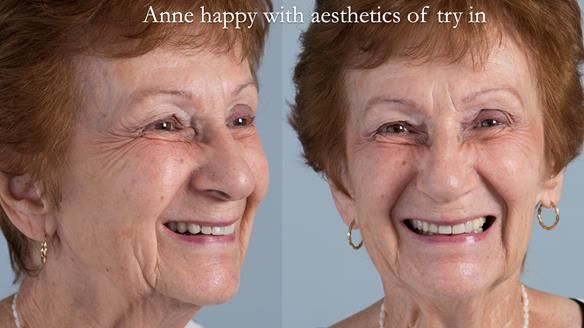
- “I really do not want to live with all this pain, anxiety and discomfort.” Finlay’s response following diagnosis - I should be able to help this with the proposed treatment plan - but I can give no absolute guarantee.
- “To be able to eat properly, not having to wonder which teeth will be coming loose next.” Finlay’s response following diagnosis - I will be able to help with this in the proposed treatment plan. It is important to understand that getting used to a denture takes time and adaption. They do not function like natural teeth, in the same way a prosthetic hand does not function in the same way a natural hand works.
- “I just want my life to be back to normal. It has been on hold for a long time now.” Finlay’s response following diagnosis - I should be able to help this with the proposed treatment plan - but I can give no absolute guarantee.
Findings/diagnoses/observations presented to the patient
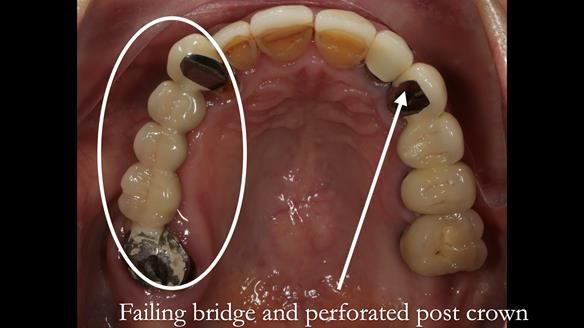
- Failing bridge in the upper right area of the mouth. The support teeth UL7 and UL3 have failed completely and require extraction. These teeth will be replaced first by an interim temporary denture, followed by a definitive cobalt chromium-based denture.
- The upper left lateral incisor tooth (UL2) has an area of infection on the tip of the root, is heavily restored, has angled post and not saveable. I recommend that this tooth is extracted and will be replaced first by an interim temporary denture, followed by a definitive cobalt chromium-based denture.
- The upper and lower teeth are worn and damaged from bruxism and acid erosion. You grind your teeth heavily, probably during sleep – “Bruxism”. The forces generated by bruxism are huge, which means that you can generate enormous forces on the teeth and are very damaging. The treatment plan set out below will help to restore your dental appearance and help to reduce the damaging forces on the remaining teeth and restorations.
- The upper left bridge (UL3, 4, 5) is weak and fragile. My first thoughts were that this needs to be extracted and replaced by a denture as part of the plan. However, with “thinking time”, I do not believe that this in your best interest as this is a useful chewing area of the mouth. The cobalt chromium-based denture described below will help to protect this bridge from bruxism. If or when the bridge fails new teeth will be able to be added onto the denture.
- The UL6 dental implant appears healthy. It is an important tooth to secure the cobalt chromium-based denture to. If this implant fails, a new denture will be required.
- The UR2, 1, UL1 have porcelain veneers on the teeth. It is impossible to predict how long these will last. The treatment plan set out below will help to protect them for as long as possible.
- The LL6 appears to have decay underneath this and has an area on the tip of the root. This requires treatment from either your general dentist or one of our specialists as the practice. Please let me know if you would like us to manage this.
- The LL4 and LL5 are linked to support the fragile LL5. This may require treatment in the future, although this impossible to predict.
- The LR1 has a root filling and is fragile. This tooth may fracture at some stage and require restoration. It is impossible to predict when this will happen. This may require treatment from either your general dentist or one of our specialists as the practice. Please let me know if you would like us to manage this.
- The LR5 and LL7 may require restoration to prevent them from chipping and breaking. This may require treatment from either your general dentist or one of our specialists as the practice. Please let me know if you would like us to manage this.
- The left jaw joint was painful to touch and sore on movement. The treatment plan below may help with this although it is impossible to guarantee that it will resolve the discomfort.
- The soft tissues of your mouth were visually screened for oral cancer. The soft tissues appeared healthy. This is a routine assessment I carry out for all of my patients.
Treatment objective for the upper teeth
- Remove upper right bridge and extract two bridge support teeth (UR7 and UR3) and extract upper left lateral incisor (UL2). Fitting of a temporary acrylic based immediate partial denture/splint.
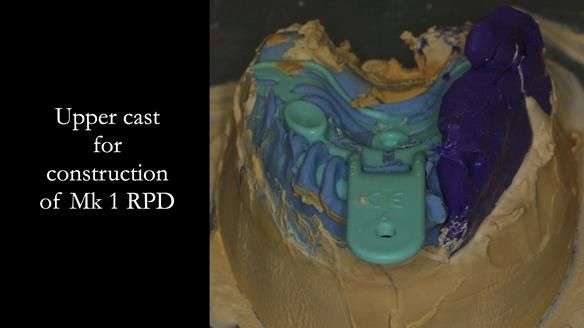
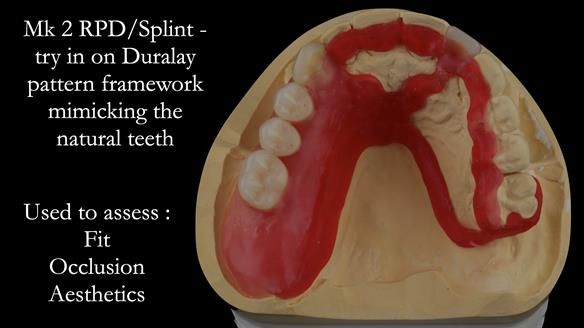
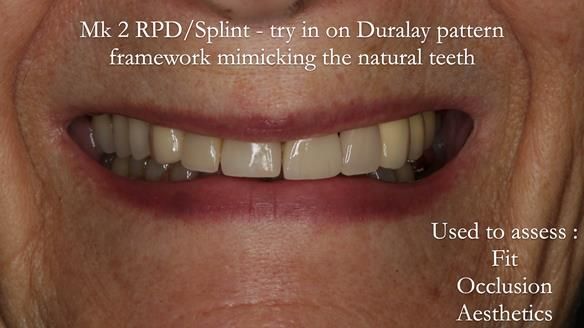
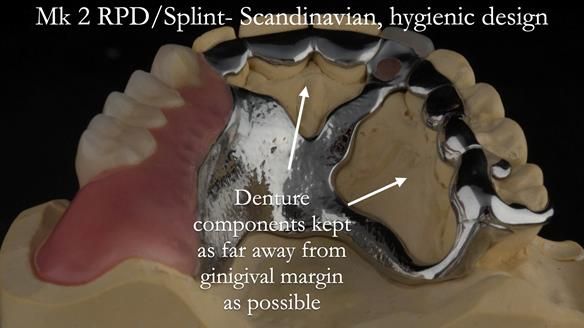
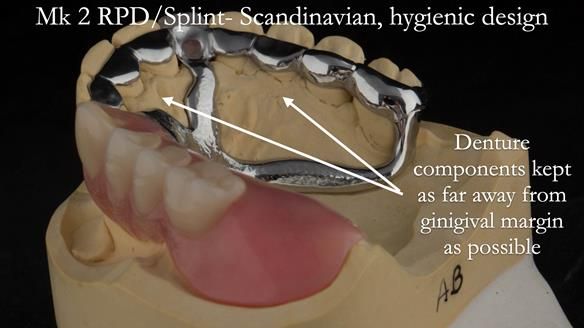
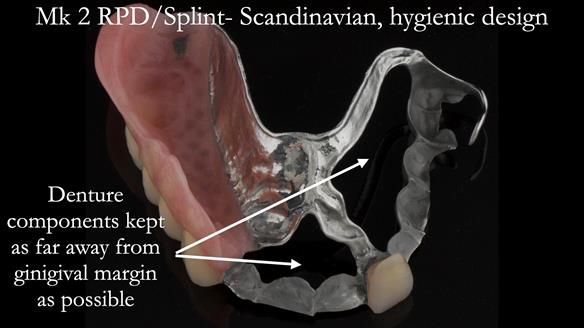
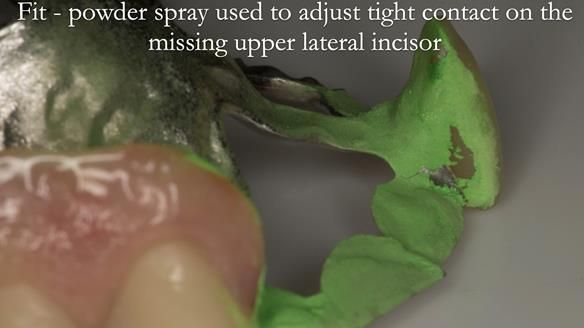
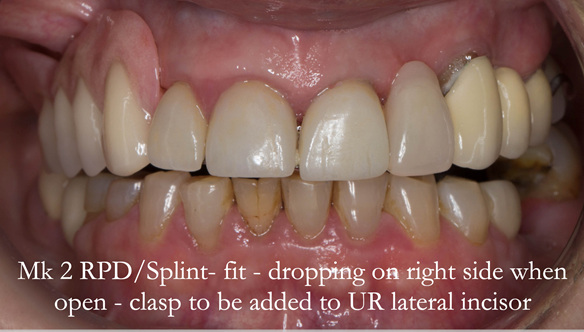
- Cobalt chromium based partial denture/splint
- Heat cured acrylic occlusal splint for night time wear
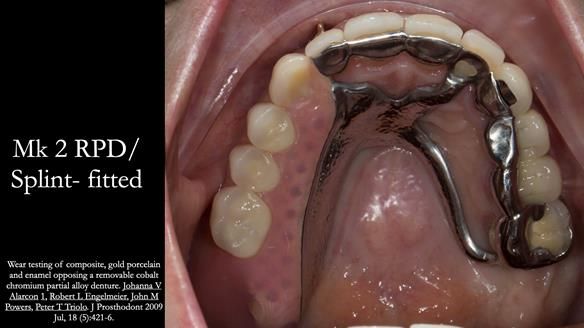
The treatment outcome was successful and fulfilled Anne’s wishes, including resolution of the temporomandibular joint pain. The opposing teeth are wear resistant to CoCr alloy on the occlusal surfaces of the RPD as per study: Wear testing of composite, gold porcelain and enamel opposing a removable cobalt chromium partial alloy denture. Johanna V Alarcon 1, Robert L Engelmeier, John M Powers, Peter T Triolo. J Prosthodont 2009 Jul, 18 (5):421-6.
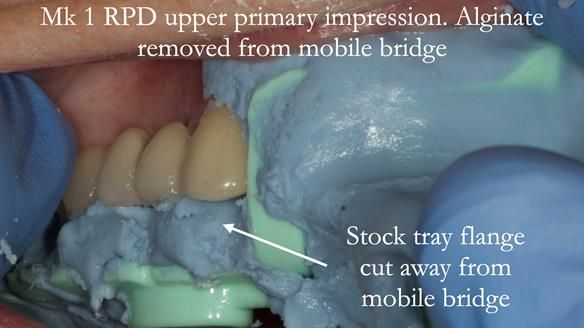
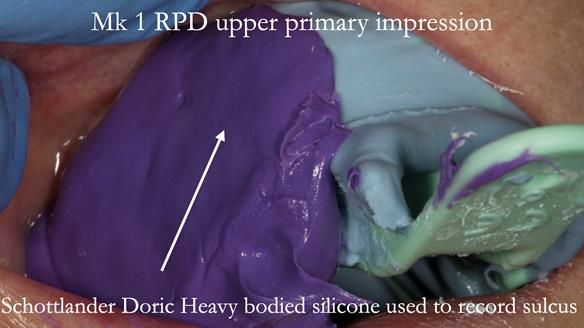
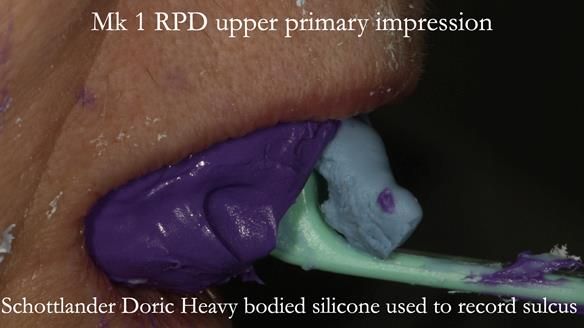
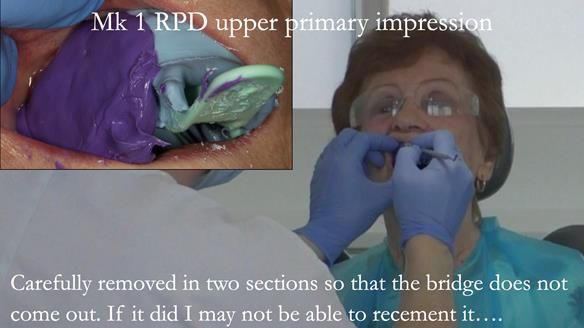
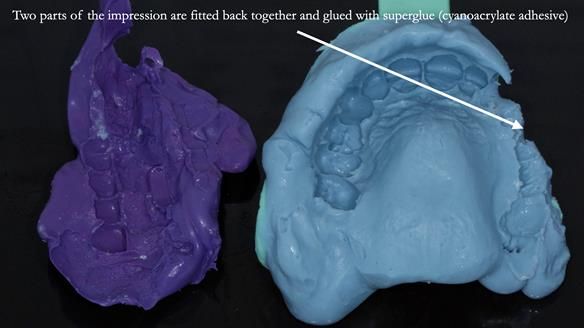
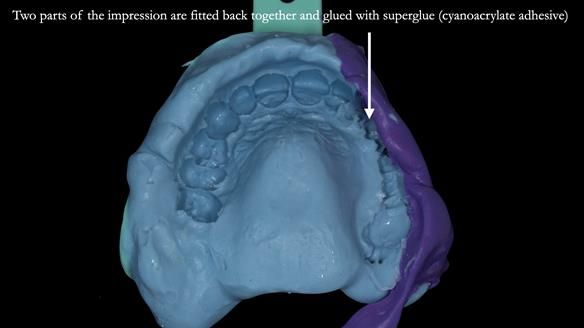
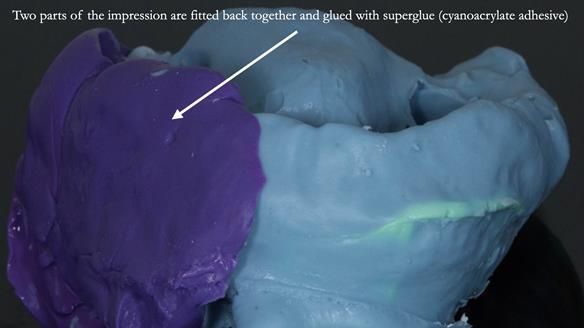
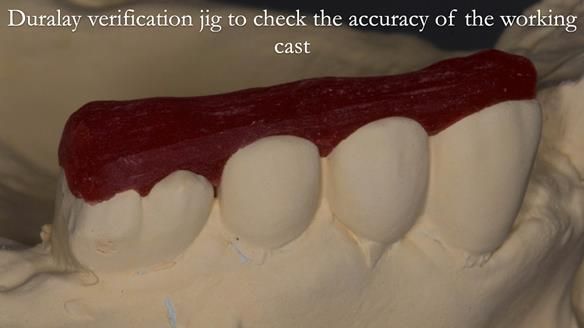
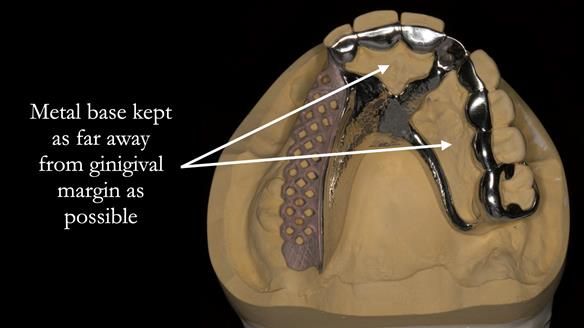
The clinical situation and treatment process is shown in detail below with photographs. I provided the clinical work. Rowan Garstang provided the technical work.
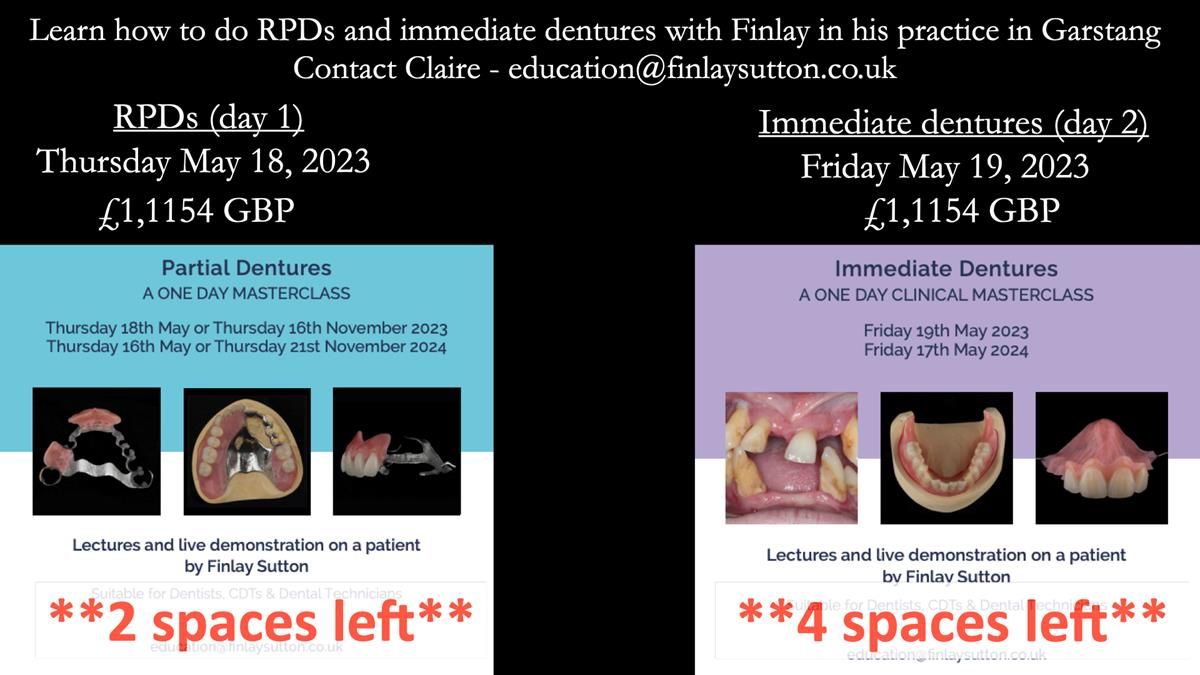
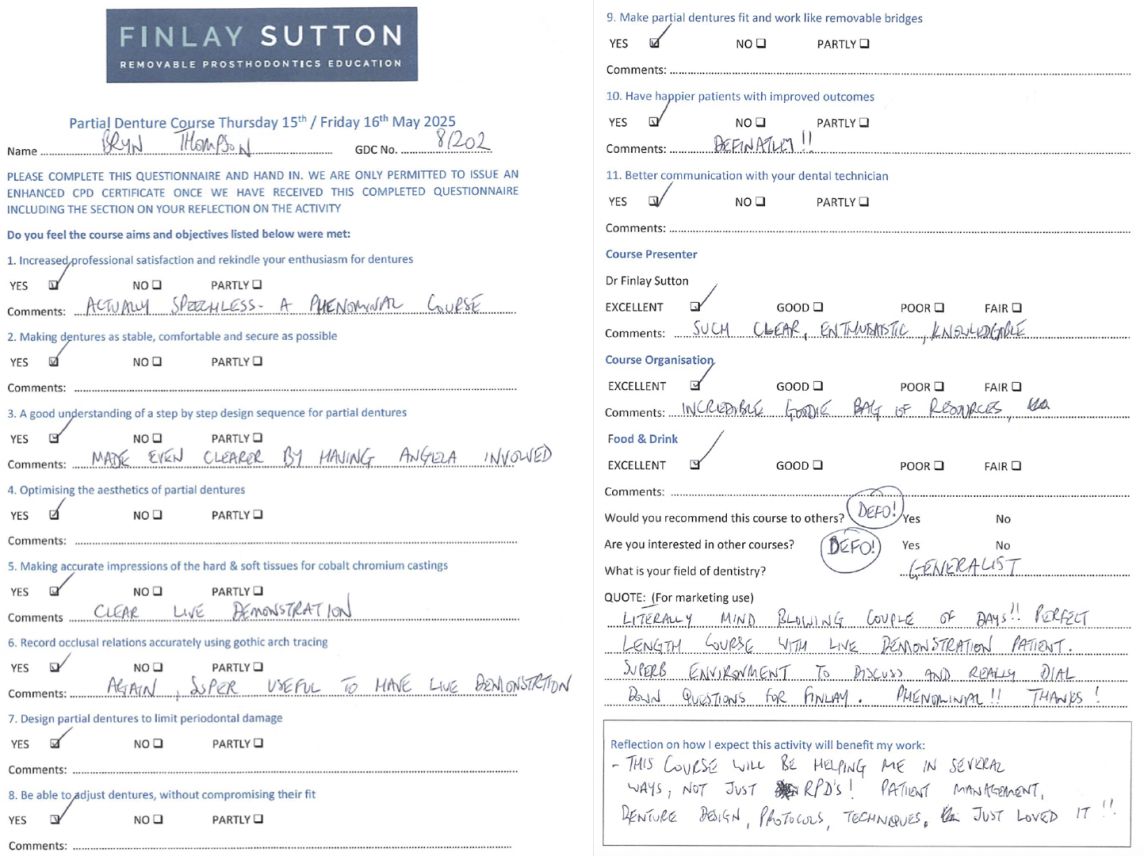
My next clinical courses at the practice in Garstang with a live patient demonstration are day 1 partial dentures (Thursday 18th May 2023 - £1,154) and day 2 immediate dentures (Friday 19th May 2023 - £1,154). These days are limited to 8 delegates per day designed for maximum interaction. These courses are aimed at general dentists, prosthodontists, clinical dental technicians and dental technicians. They are completely clinical, demonstrating how to provide dentures which have optimal function and superb aesthetics. I give live patient demonstrations along with lectures abundantly illustrated with step-by-step photographs and videos of all procedures. Delegates will take many “nuggets of gold”, being able to put the advice straight into practice with immediate improvement in professional satisfaction and patient outcomes.
If you enjoy my Newsletters and you have friends, colleagues, dental students, dental technicians, clinical dental technicians and postgraduate dentists that you think will appreciate them, please feel free to share them. In addition, if you or your colleagues would like to receive my Newsletters, please email me (education@finlaysutton.co.uk) and I will update the list.
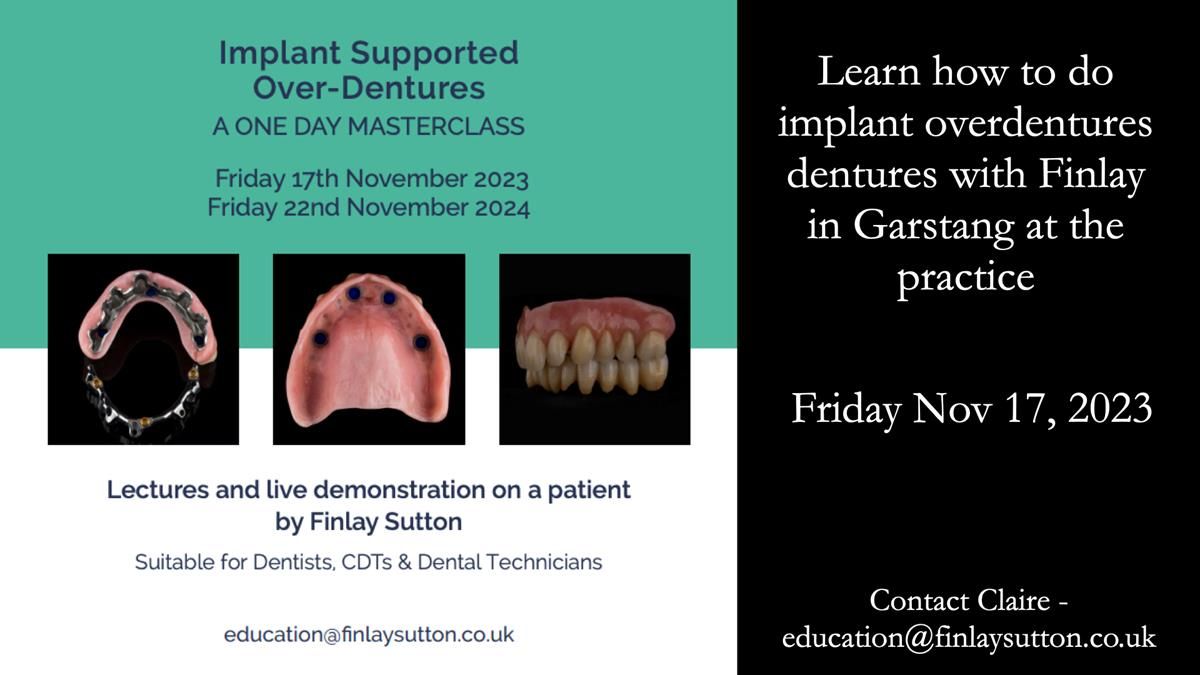
Please see details of courses and lectures (in UK and rest of the world) to be given by Finlay over during 2023 at the end of this Newsletter
education@finlaysutton.co.uk
Subscribe to Newsletter
Information about Finlay's In-House Courses
Information about Finlay's speaking engagements